The 2017 EULAR/ACR classification criteria for adult and juvenile idiopathic inflammatory myopathies
| Variable | Score Points | Definition | |
| Without muscle biopsy | With muscle biopsy | ||
| Age of onset | |||
| Age of onset of first symptom assumed to be related to the disease ≥ 18 years and < 40 years | 1.3 | 1.5 | 18 ≤ Age (years) at onset of first symptom assumed to be related to the disease < 40 |
| Age of onset of first symptom assumed to be related to the disease ≥ 40 years | 2.1 | 2.2 | Age (years) at onset of first symptom assumed to be related to the disease ≥ 40 |
| Muscle weakness | |||
| Objective symmetric weakness, usually progressive, of the proximal upper extremities | 0.7 | 0.7 | Weakness of proximal upper extremities as defined by manual muscle testing or other objective strength testing, which is present on both sides and is usually progressive over time |
| Objective symmetric weakness, usually progressive, of the proximal lower extremities | 0.8 | 0.5 | Weakness of proximal lower extremities as defined by manual muscle testing or other objective strength testing, which is present on both sides and is usually progressive over time |
| Neck flexors are relatively weaker than neck extensors | 1.9 | 1.6 | Muscle grades for neck flexors are relatively lower than neck extensors as defined by manual muscle testing or other objective strength testing |
| In the legs proximal muscles are relatively weaker than distal muscles | 0.9 | 1.2 | Muscle grades for proximal muscles in the legs are relatively lower than distal muscles in the legs as defined by manual muscle testing or other objective strength testing |
| Skin manifestations | |||
| Heliotrope rash | 3.1 | 3.2 | Purple, lilac-colored or erythematous patches over the eyelids or in a periorbital distribution, often associated with periorbital edema |
| Gottron´s papules | 2.1 | 2.7 | Erythematous to violaceous papules over the extensor surfaces of joints, which are sometimes scaly. May occur over the finger joints, elbows, knees, malleoli and toes |
| Gottron’s sign | 3.3 | 3.7 | Erythematous to violaceous macules over the extensor surfaces of joints, which are not palpable |
| Other clinical manifestations | |||
| Dysphagia or esophageal dysmotility | 0.7 | 0.6 | Difficulty in swallowing or objective evidence of abnormal motility of the esophagus |
| Laboratory measurements | |||
| Anti-Jo-1 (anti-histidyl-tRNA synthetase) autoantibody present | 3.9 | 3.8 | Autoantibody test in serum performed with standardized and validated test, showing positive result |
| Elevated serum levels of creatine kinase (CK)* or lactate dehydrogenase (LDH)* or aspartate aminotransferase (ASAT/AST/SGOT)* or alanine aminotransferase (ALAT/ALT/SGPT)* | 1.3 | 1.4 | The most abnormal test values during the disease course (highest absolute level of enzyme) above the relevant upper limit of normal |
| Muscle biopsy features- presence of: | |||
| Endomysial infiltration of mononuclear cells surrounding, but not invading, myofibres | 1.7 | Muscle biopsy reveals endomysial mononuclear cells abutting the sarcolemma of otherwise healthy, non-necrotic muscle fibers, but there is no clear invasion of the muscle fibers | |
| Perimysial and/or perivascular infiltration of mononuclear cells | 1.2 | Mononuclear cells are located in the perimysium and/or located around blood vessels (in either perimysial or endomysial vessels) | |
| Perifascicular atrophy | 1.9 | Muscle biopsy reveals several rows of muscle fibers which are smaller in the perifascicular region than fibers more centrally located | |
| Rimmed vacuoles | 3.1 | Rimmed vacuoles are bluish by Hematoxylin and Eosin staining and reddish by modified Gomori- Trichrome stains | |
*Serum levels above the upper limit of normal
**This classification criteria can be used only when no better explanation for the symptoms and signs exists
Table adapted from Lundberg IE, et al. 2017 European League Against Rheumatism/American College of Rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups.
The score can be converted into a probability of IIM (Figure 1A, B) by:
| Probability of IIM including muscle biopsy =1/[1+exponential(5.33–score)] |
OR
| Probability of IIM without muscle biopsy =1/[1+exponential(6.49−score)] |
or by utilizing the online web-calculator (www.imm.ki.se/biostatistics/calculators/iim).
Classification tree for subgroups of idiopathic inflammatory myopathies (IIM)
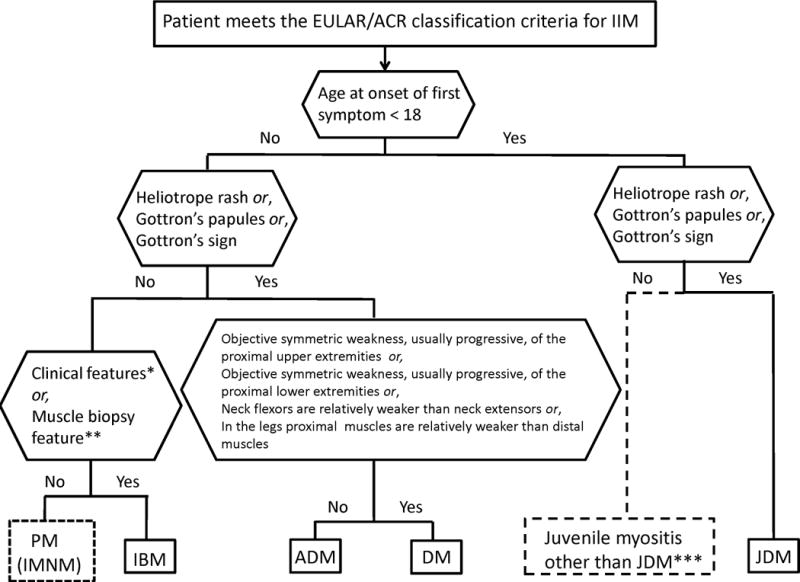
Classification tree for subgroups of idiopathic inflammatory myopathies (IIM). A patient must first meet the EULAR/ACR classification criteria for IIM (probability of IIM ≥55%). The patient can then be sub-classified using the classification tree. The subgroup of PM patients includes patients with immune-mediated necrotizing myopathy (IMNM). For IBM classification one of the following, *Finger flexor weakness and response to treatment: not improved, or **Muscle biopsy: rimmed vacuoles, is required for diagnosis. ***Juvenile myositis other than JDM was developed based on expert opinion. IMNM and hypomyopathic DM were too few to allow sub-classification.
PM, polymyositis; IMNM, immune-mediated necrotizing myopathy; IBM, inclusion body myositis; ADM, amyopathic dermatomyositis; DM, dermatomyositis; JDM, juvenile dermatomyositis.
